Article attribution to Mike Miesen, a volunteer in Uganda who is working with the Kissito Healthcare International initiative to reduce maternal mortality at the Mbale Regional Referral Hospital.
Let’s just get this out of the way: With two years left, it is highly unlikely that Millennium Development Goal (MDG) 5a – in the clunky verbiage of the UN: “Reduce by three quarters, between 1990 and 2015, the maternal mortality ratio” – will be met worldwide.
But substantial progress has been made, which, in human terms, means that hundreds of thousands of maternal deaths have been prevented. It’s worth taking a step back to understand the scope and scale of the problem, and to think through the interventions that have been successful in myriad developing and developed countries.
The Maternal Mortality Ratio (MMR) is calculated as the number of pregnancy-related deaths (from any point in the pregnancy to 42 days post-birth/termination) per 100,000 live births. In 2010, an estimated 287,000 mothers died from pregnancy-related causes, or 210 deaths per 100,000 live births; it’s an almost 50 percent reduction from 1990, when an estimated 543,000 mothers died, or 400 per 100,000 live births.
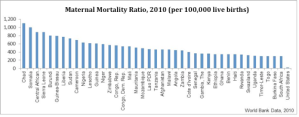
These roll-up figures mask a wide variation in the distribution of maternal mortality; in 2010, an astounding 99% of deaths occurred in the developing world (56% in sub-Saharan Africa alone), and the MMR in developing countries is, on average, 15 times higher than in developed countries. According to the World Bank, the country with the highest MMR in 2010 was Chad, the lowest Estonia, at 1,100 and 2 per 100,000 live births, respectively. A chart showing the 40 countries with the highest MMR is below, with the United States – at 21 – added for reference:
Scan the list of countries and it becomes clear that the MMR problem is clustered in Africa, with few exceptions; there’s wide variation among developing countries, too. The question is: why?
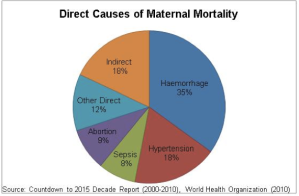
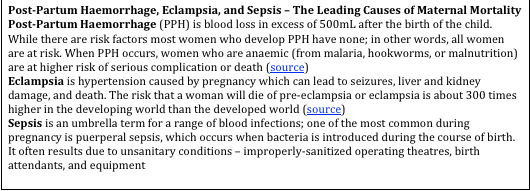
Worldwide, the leading direct causes of maternal mortality are Post-Partum Haemorrhage (PPH); Pre-eclampsia and eclampsia; and sepsis (see Figure X). Together, these three conditions account for 60% of maternal deaths. At the patient-level, interventions to prevent or treat all three are well-understood, cheap, and straightforward:
- Prevention of PPH is facilitated by following a protocol known as Active Management of the Third Stage of Labor (AMTSL), which involves the administration of an uterotonic (e.g., oxytocin, ergometrine, misoprostol) and massaging/monitoring for two hours post-birth. A Randomized Controlled Trial (RCT) found that women who received AMTSL experienced PPH 6.8% of the time vs. 16.5% with passive/conservative management – almost a 60% decrease
- Treatment of pre-eclampsia and eclampsia involves the injection of magnesium sulphate, a cheap compound (in the West, the non-pharmaceutical preparation is known as Epsom salt). A highly-regarded RCT found that magnesium sulphate halves the risk of eclampsia in pregnant women
- Prevention of puerperal fever*, or sepsis more generally, is a matter of maintaining proper sanitation before, during, and after a birth. If a mother develops sepsis, a full course of antibiotics can be administered as treatment
Here’s what’s clear: the devil isn’t in the details – it’s in the diffusion of pharmaceuticals, health care workers, and knowledge through health systems, and in improving those systems holistically. It goes deeper than the health system, of course; to administer AMTSL, for example, requires the drug being available (partially a supply chain/regulation issue), a health care worker who is trained to administer the drug (an education issue), and a health care worker who has the time to administer the massage every 15 minutes for two hours (a financing issue). And keep in mind: that’s only if the mother has a trained health care worker by her side, which in sub-Saharan Africa puts her in the minority, with only about 46% of births attended by skilled health personnel in 2008.
The complex task of reducing maternal mortality demands a multifactorial solution that draws on a wide coalition of government departments and private organizations – and each country has to find a solution that meshes with its own cultural and structural realities. Nevertheless, there are broad themes that transcend these inter-country differences and show up in the success stories of many positive deviants:
- Increase access to family planning and contraception
- Strengthen demand for antenatal check-ins through education campaigns, conditional cash transfer programmes, or easier access to skilled professionals
- Increase the percentage of births attended to by a skilled professional; ensure skilled professional is able to provide necessary care (e.g., equipment, pharmaceuticals, knowledge) for non-complicated birth and is able to refer complicated cases
- Ensure Emergency Obstetric and Neonatal Care (EmONC) services are comprehensive and of high quality, and that health centres are staffed with skilled workers; stocked with maternal medicines, antibiotics, and proper equipment; and accessible to remote populations
- Establish or strengthen monitoring systems to highlight successes and areas of opportunity
All of which goes a long way towards our understanding of why some countries have already reached MDG 5a and others are unlikely to do so: the interventions require sustained political will, ‘soft’ infrastructure (e.g., regulations, communication), consistent funding, and a systems approach to process improvement. Unfortunately, it may take more than 20 or 25 years to build out this basic scaffolding on which to build sustainable change.
The imminent failure to reach the goal of reducing the MMR by 75% by 2015 shouldn’t obscure the fact that there are hundreds of thousands of mothers alive who, without the focus on maternal mortality, may not be otherwise. Much more can – and will – be done in the next two years, and in the next two decades.
In many ways, 2015 is just the start.
*If you’re a public health or history of medicine wonk, you may recall that puerperal fever (or childbed fever, as it was known) was the disease that led Ignaz Semmelweis to call for basic hygiene measures in his Viennese hospital pre-Germ Theory of Disease – and was promptly rejected from the establishment for his heresy. As one contemporary doctor put it, “Doctors are gentlemen, and gentlemen’s hands are clean.”